TL;DR:
Prostate biopsies are essential in diagnosing prostate cancer by extracting tissue samples for analysis. Different biopsy methods vary in accuracy and side effects. MRI-targeted biopsies offer improved accuracy over traditional TRUS biopsies. Preparation and recovery involve simple steps, and early detection is crucial for successful treatment.
Main points:
- Prostate biopsies confirm cancer diagnoses after initial screening.
- MRI-guided biopsies are more accurate than TRUS biopsies.
- Preparation includes stopping certain medications and taking antibiotics.
- Biopsies are outpatient procedures usually with minimal recovery time.
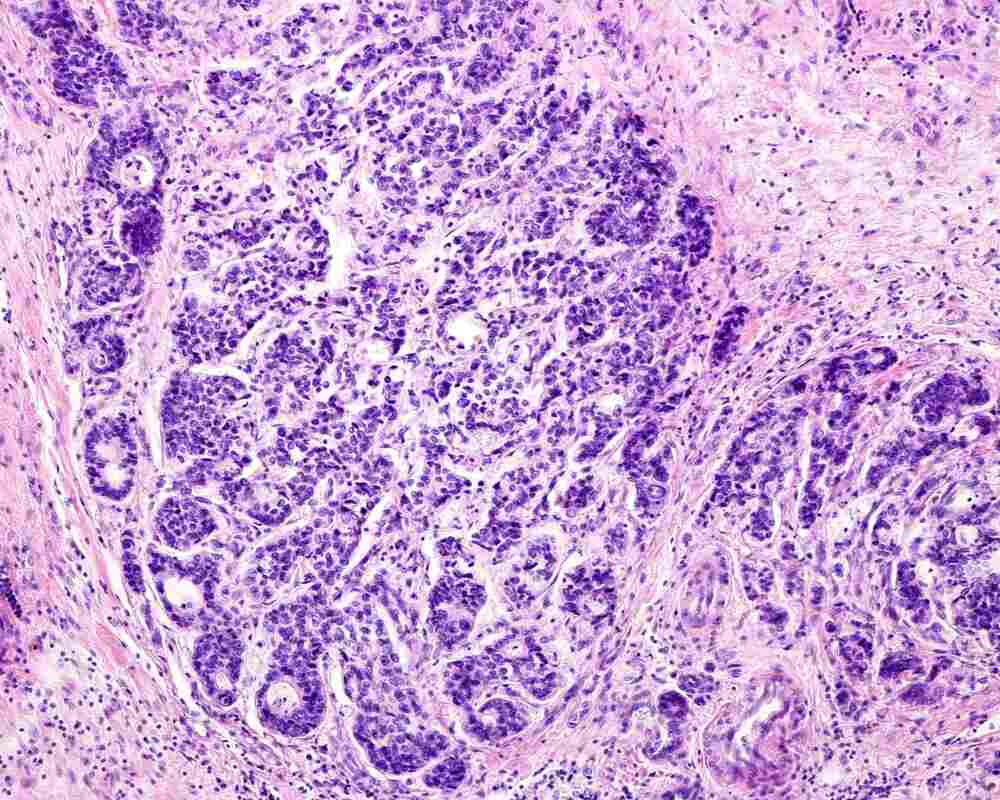
Prostate biopsies play an important role in helping physicians diagnose cancer in the prostate gland. By taking a tissue sample and analyzing it, pathologists can identify cancerous cells and grade their severity. In turn, patients and their physicians can make more informed decisions about the need for treatment and how to move forward.
Prostate biopsy results are only one part of a larger diagnostic process. Additionally, not all forms of prostate biopsy are equally effective in identifying the presence of prostate cancer. However, accurate methods for prostate biopsy are available and widely used to help patients.
Keep reading to learn more about prostate biopsies, including what happens during the procedure and what sets different types of prostate biopsies apart.
The Role and Importance of Prostate Biopsies in Identifying Prostate Cancer
A biopsy is a common diagnostic procedure. It is frequently used to identify various cancers as well as diagnose a range of other conditions and disorders.
Physicians and other healthcare professionals involved need a great amount of education and experience to safely perform a biopsy, correctly analyze it, and accurately interpret the results. However, the basic idea behind a biopsy is simple: a sample of cells or tissue is extracted from the body and then analyzed.
Prostate Exams and Biopsies: Why Prostate Biopsies are Essential
For prostate cancer specifically, a prostate biopsy is used for confirmation when earlier screening tests indicate the potential presence of cancer.
For example, prostate-specific antigen (PSA) testing measures the level of a specific protein produced by the prostate in blood. High PSA levels can indicate the presence of prostate cancer.
However, a high PSA level can also indicate other conditions, such as benign prostatic hyperplasia (BPH) or prostatitis (inflammation of the prostate). High PSA levels can also result from a variety of activities and other circumstances. While PSA testing can guide physicians toward further testing and a diagnosis, it cannot confirm the presence of prostate cancer.
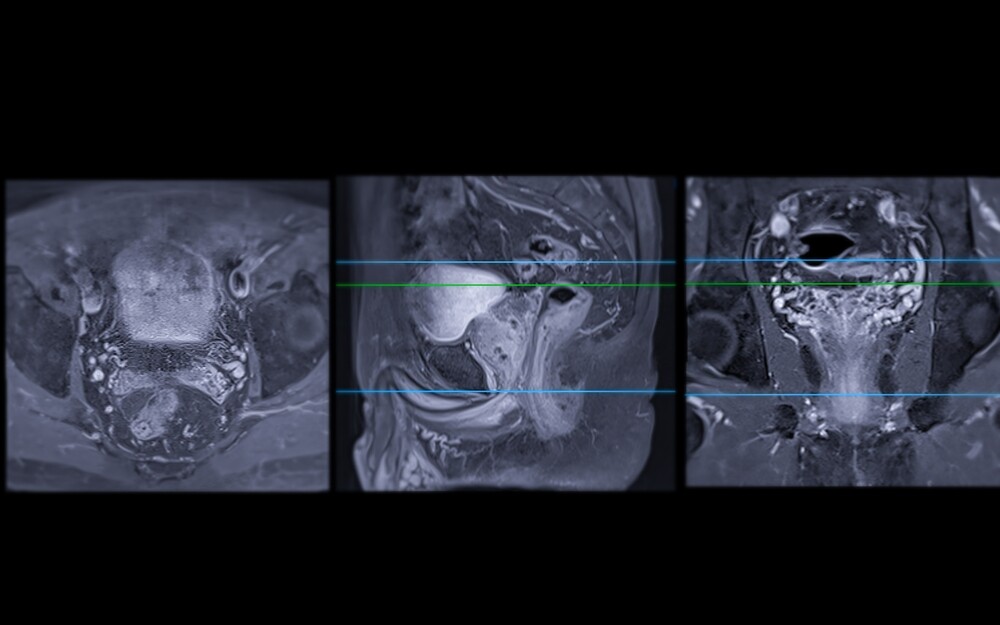
The same is true of MRI diagnostics for prostate cancer. Peer-reviewed research published in the Canadian Medical Association Journal explains that MRI substantially outperforms trans-rectal ultrasound (TRUS) biopsy, a systematic but non-targeted form of biopsy, as a diagnostic tool. MRI guided biopsies accurately diagnosed prostate cancer in 93% of cases, compared to 48% for TRUS biopsies.
However, even when MRI is used, a biopsy is still required to confirm the presence of cancer. MRI enables radiologists to identify areas where prostate cancer is likely present, and depending on how it is used, it can guide the biopsy needle into the lesion. The prostate biopsy procedure itself is needed to provide the tissue sample that leads to a conclusive prostate cancer diagnosis.
Prostate Biopsy and Early Detection
While biopsies themselves are not frontline diagnostic tools, they are crucial for confirming the presence of prostate cancer. Routine prostate cancer screenings support early detection, and biopsies provide further evidence needed to move on to treatment.
The American Cancer Society explains that, when prostate cancer is contained to the prostate or has only spread to nearby areas, the five-year relative survival rate is greater than 99%. However, the five-year relative survival rate when prostate cancer spreads to more distant parts of the body is only 34%.
Early detection, ultimately including a prostate biopsy to confirm diagnosis, is crucial for catching prostate cancer before it has spread throughout the body.
What to Expect During the Prostate Biopsy Process
As mentioned previously, there are several types of prostate biopsies used to diagnose prostate cancer. We will explore a few of these procedures in the following section. This section reviews the prostate biopsy process in general, including how to prepare and what to expect.
Common screening procedures that lead to a prostate biopsy include PSA tests and digital rectal exams (DREs). Next steps can include an MRI, transrectal ultrasound, or biopsy, as the Mayo Clinic explains.
As previously noted, MRI-guided biopsies greatly outperform TRUS biopsies, which are systematic but blind, in detecting prostate cancer. In other words, TRUS biopsies collect samples without using imaging guidance to direct the biopsy needles toward areas suspected of containing cancerous cells.
With that in mind, consider this information on preparing for a biopsy and a review of what happens during the procedure.
Prostate Biopsy Preparation
Always follow the specific directions your healthcare provider shares with you when preparing for a biopsy. That said, common practices when preparing for a prostate biopsy include, as Mount Sinai Hospital explains:
- Ceasing use of certain medications and supplements, such as blood thinners and certain anti-inflammatory drugs.
- Performing an at-home enema before the procedure.
- Eating less than normal the day before the biopsy.
- Taking a preventative course of antibiotics.
The Prostate Biopsy Procedure Itself
A prostate biopsy is a common outpatient procedure, taking roughly a half-hour. The process can be uncomfortable to a degree and is sometimes painful.
Physicians use a local or general anesthetic to address pain during the procedure. Then, they insert a thin needle into the prostate, either through the rectum or the perineal area, to collect tissue samples. The next section of this blog explains different types of prostate biopsies in more detail.
Following the biopsy, a physician may recommend avoiding heavy activity for a day or two. Patients may be reminded to continue their course of antibiotics, and they may notice soreness, bleeding, and/or the presence of blood in urine, stool, or semen.
Serious side effects are not particularly common but are possible. The side effects of prostate biopsies include bruising and pain at the biopsy site, bleeding, infection, and issues with urination, as Johns Hopkins explains.
Patients can also develop a serious infection from the biopsy and require IV antibiotics, and possibly even be admitted to the hospital. The results of a study published in the peer-reviewed Journal of Urology show that roughly 2.5% of patients experienced an infection after a prostate biopsy. Additionally, peer-reviewed research published in the journal Urology found that, as of 2015, 1.3% percent of patients experience post-biopsy infections that require hospitalization.
Understanding Common Types of Prostate Biopsies
There are several types of prostate biopsy procedures used to determine a prostate cancer diagnosis. These include:
Transrectal Ultrasound-Guided Biopsy (TRUS)
TRUS biopsies use an ultrasound probe inserted into the anal cavity to produce an image of the prostate and the area around it. Using this image, the physician will then take tissue samples from the prostate for examination by inserting a biopsy needle through the rectum.
While the selection of biopsy sites is guided by imaging, the samples are ultimately taken randomly, usually one from somewhere within each of the twelve segments of the prostate. Peer-reviewed research published in The Lancet found that clinically significant prostate cancer was detected in 48% of instances where patients had clinically significant prostate cancer. In other words, 52% of patients who had a clinically significant prostate cancer were told that the biopsy did not find any cancer or any clinically significant cancer but were wrong!
TRUS biopsies generally take 12 random tissue samples. Each biopsy site represents the potential for side effects and complications. Combined with the random nature of sampling, TRUS biopsies can lead to increased risks for patients.
Transperineal Biopsy
Transperineal biopsies are sometimes similar to TRUS biopsies in that they both involve the use of a rectal probe to generate imaging of the prostate and the area around it. In other instances, transperineal biopsies use MRI imaging to better identify abnormal areas and direct the selection of biopsy samples.
The major and consistent difference between the two procedures is how the biopsy needle enters the body. In a transperineal biopsy, the needle passes through the perineal wall — the area between the anus and testicles.
Medscape explains that this approach offers similar results as a TRUS biopsy in terms of detecting cancer, but reduces the risk for infection. Even when detection rates are similar, safer procedures are always preferable.
MRI-Targeted Biopsy
MRI-guided biopsy uses detailed imaging before and during the procedure, generated by a multiparametric MRI (mpMRI) machine, to better guide the selection of samples. As compared to ultrasound and even to standard MRI, mpMRI offers more information about abnormal areas of the prostate to physicians.
With more detail available to physicians, taking samples from specific areas of concern within the prostate becomes easier. A peer-reviewed study published in The New England Journal of Medicine found mpMRI led to the detection of clinically significant cancer in 38% of patients in the study, as compared to 26% for standard ultrasound biopsy.
The improved accuracy of MRI-targeted prostate biopsy offers two key advantages:
- Patients with elevated PSA levels, but previous negative results from a TRUS biopsy, can benefit from the increased accuracy of MRI-targeted biopsy. Detailed imaging and enhanced guidance for biopsy selection can provide a more accurate result in terms of identifying cancer.
- All patients can benefit from the improved imaging. While a biopsy is still needed to conclusively diagnose prostate cancer, the improved selection of areas to take samples from can lead to improved accuracy in that diagnosis.
Moving Forward with Prostate Biopsies
Biopsies are not frontline tests or diagnostics — they should only be used when preliminary tests indicate the potential for prostate cancer. That said, patients who have a biopsy recommended to them by their physician should consider their options, including an approach that offers increased accuracy.
Prostate Laser Center is committed to diagnosing and treating prostate cancer with minimally invasive options that have a reduced risks for side effects as compared to more traditional treatments.
Seeking treatment for prostate cancer? Schedule a consultation.
NOTE: The information provided on this website is general medical information and does not establish a physician-patient relationship. Please discuss your particular situation with a qualified medical professional.