Are you interested in learning more about treatment options for prostate cancer? There are many options used to treat prostate cancer, depending on the stage and spread of the cancer.
Examples of treatment options include watchful waiting, active surveillance, medication, surgery such as radical prostatectomy, radiation, focal laser therapy, and ultrasound therapy. In this article, we focus on a minimally invasive procedure for partial gland and whole gland treatment: Transurethral ultrasound ablation (TULSA-PRO).
TULSA-PRO utilizes therapeutic ultrasound to ablate prostate tissue showing signs of cancer. In simpler terms, the ultrasound energy destroys cancerous tissue in the prostate.
Real-time MRI imaging and temperature mapping offer valuable support during this procedure. With visual and thermal feedback, physicians can precisely direct the thermal ultrasound energy to treat cancer while sparing surrounding healthy tissue.
Keep reading to learn more about TULSA treatment for prostate cancer. We will explain what prostate cancer is and share more information about TULSA-PRO. That includes TULSA prostate treatment success rate and data about the incidence of side effects.
What is Prostate Cancer?
Understanding the Prostate Gland
The prostate itself is a small gland that sits below the bladder and surrounds the urethra. This small gland, roughly the size of a walnut when healthy, is part of the male reproductive system.
The prostate gland contributes fluid to help support and protect sperm. It also helps to move that fluid into the urethra during ejaculation.
Basic Information on Prostate Cancer
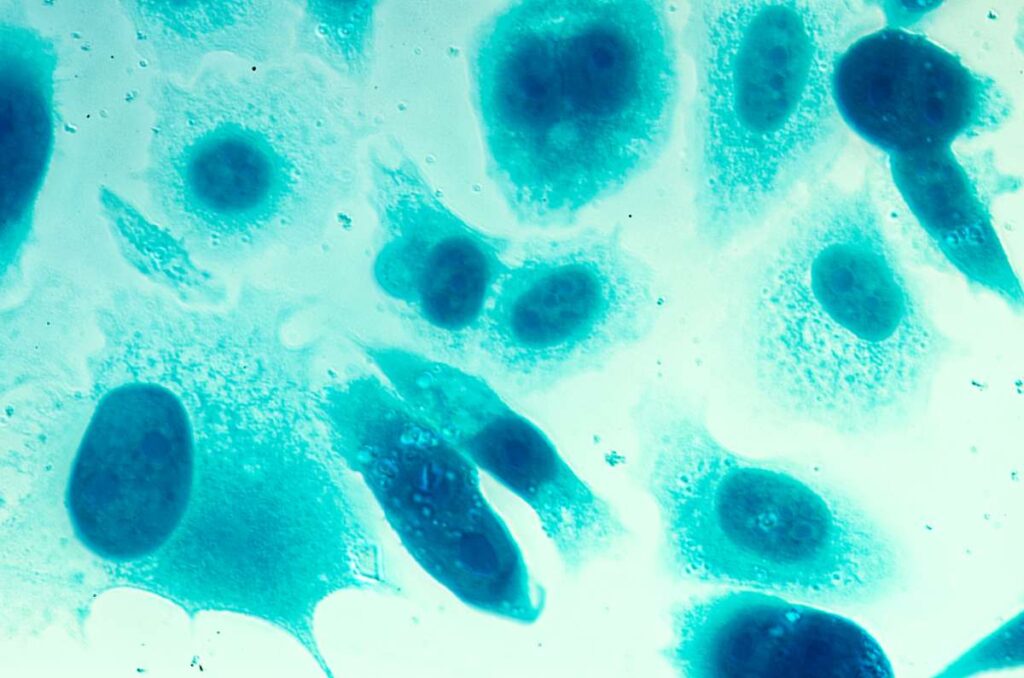
Prostate cancer is an abnormal, uncontrolled growth of cells in the prostate, the American Cancer Society explains. Many instances of prostate cancer are slow to develop, meaning they require only minimal treatment.
Risk factors for prostate cancer include age, family history, and genetic mutations inherited at birth. There are several potential avenues for reducing the risk of prostate cancer. However, these actions cannot eliminate the risk of prostate cancer.
However, prostate cancer can also grow more aggressively. In these cases, the risk of the cancer spreading to other parts of the body can increase. More aggressive prostate cancer requires more proactive treatment.
Prostate cancer may have no signs or symptoms in its early stages, the Mayo Clinic explains. As this disease advances, symptoms related to difficulty with urination can appear.
Weak or intermittent flow and a frequent need to urinate are two examples. Blood in urine or semen and erectile dysfunction can also occur.
Treatments for prostate cancer depend on the cancer’s aggressiveness and spread, the patient’s ability to recover from a specific treatment, and other factors.
Active treatment options range from the minimally invasive, like the TULSA prostate procedure and laser focal therapy, to more invasive options like surgery. Medication, cryotherapy, radiation therapy, and other treatments are also used.
Let’s look more closely at TULSA-PRO prostate cancer treatment.
What is the TULSA Procedure?
TULSA-PRO is a minimally invasive outpatient procedure that utilizes ultrasound to generate increased temperatures. That heat then destroys (ablates) cancerous tissue in the prostate.
TULSA-PRO is FDA-cleared and does not require any incisions or the use of radiation. It can more easily target a broader area than focal laser therapy, offering a potential treatment option for patients with larger or more diffuse cancers within the prostate.
A rod-shaped device that emits ultrasound energy is the foundation of the TULSA treatment for prostate cancer. The device is inserted into the urethra. It then emits directional ultrasound as directed by the physician.
Profound Medical, the developer of the TULSA prostate procedure, explains this approach helps to spare nerve tissue and the external urethral sphincter which are just outside the prostate. Ablating cancerous tissue through the urethra reduces contact with the neurovascular bundles around the prostate.
Because those nerve bundles and the external urinary sphincter support the important functions of erections and urinary continence, this approach can help to reduce the potential for side effects following treatment compared with surgery. Clinical research used to support Profound Medical’s FDA clearance application included data that found only a 7% incidence of urinary incontinence among the study population of 115 individuals after a period of 12 months.
Crucially, real-time MRI guidance and temperature mapping help to keep the physician informed of the state of the area being treated as well as the surrounding tissue. This real-time data guides the process and focuses treatment on the cancerous cells. Cooling mechanisms also help to protect non-cancerous tissue surrounding the treatment area.
TULSA Prostate Treatment Success Rate
Efficacy is a pivotal consideration when it comes to prostate cancer treatment options. What does the success rate for TULSA prostate treatment look like?
A study published in The Journal of Urology found that, after one year, 85% of 111 study participants were free of cancer scoring in Gleason Grade Group 2 (GG2) or above. Additionally, 79% of participants were free of GG2 and high-volume GG1 disease. These statistics are two ways to express TULSA prostate treatment success rate
Grade Groups help to describe how cancer may behave and progress, as Mount Sinai explains. Grade Group 2 and 3 represent medium-grade cancer, while Grade Group 1 represents low-grade cancer.
A retrospective evaluation published in The Journal of Urology found that, among 180 patients treated using TULSA-PRO:
- 98% of men treated preserved continence without the use of continence pads.
- No men treated experienced bowel-related complications.
- All men (100%) who had erectile potency before treatment maintained that potency following treatment.
The study concluded: “Lesion-targeted TULSA is a safe and customizable prostate ablation therapy with promising mid-term oncological outcomes and minimal side-effect profile on patients erectile, bowel, and urinary functions.”
The research data presented by Profound Medical indicates that the TULSA procedure for prostate cancer has favorable incidence rates for side effects. That’s as compared to prostatectomy, radiation treatment, and high-intensity focused ultrasound (HIFU) treatment.
TULSA-PRO demonstrated a 20-25% incidence of erectile dysfunction and a 2.6% incidence of moderate to severe urinary incontinence. According to this data, erectile-related side effects with TULSA-PRO occur significantly less frequently than with the three other treatment options mentioned. TULSA-PRO also leads to a notably lower rate of urinary incontinence as compared to a prostatectomy.
How Much Does the Tulsa Procedure Cost?
Prostate Laser Center charges $31,000 for the TULSA prostate procedure as of October 2023.
Accessing Treatment for Prostate Cancer
Prostate Laser Center offers effective, minimally invasive treatment options for prostate cancer and benign prostatic hyperplasia (BPH), including TULSA-PRO and focal laser therapy. A consultation with a physician is the first step in building a treatment plan to address your individual situation.
Ready to learn more about potentially treating prostate cancer with TULSA-PRO or laser focal therapy? Request a consultation today.
NOTE: The information provided on this website is general medical information and does not establish a physician-patient relationship. Please discuss your particular situation with a qualified medical professional.