Benign prostatic hyperplasia (BPH) is a common condition among older men. While generally not life-threatening, BPH can lead to serious discomfort and a range of complications.
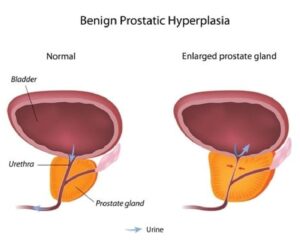
BPH is another term for an enlarged prostate. When the prostate gland grows too large, it can disrupt normal functions of the urethra and bladder. Symptoms include difficulty urinating and incomplete bladder emptying.
A variety of standard treatments are currently in use to treat BPH. Although they have effective results, they can also frequently lead to complications and unwanted side effects.
MRI-guided laser prostate ablation is emerging as a new and effective treatment for BPH. Pioneered by physicians including Dr. Ara Karamanian of the Prostate Laser Center, this treatment is less invasive than traditional options and can offer a lower incidence of side effects.
Keep reading to learn more about BPH, standard treatments, and MRI-guided prostate laser ablation. Building an understanding of treatment options and BPH itself can help you make a more informed decision about your health.
What is BPH? Definition, Diagnosis, Symptoms, and More
Benign prostatic hyperplasia, sometimes called benign prostate enlargement, is a condition that affects the prostate. The prostate itself is a gland found underneath the bladder and in front of the rectum. The urethra passes through a part of the prostate called the transitional zone.
In general, the prostate grows as men age. BPH refers to excessive growth of transitional zone prostate tissue. An enlarged prostate can lead to noticeable symptoms and negative effects on quality of life.
Most BPH symptoms are related to difficulties with urination. As prostate tissue grows, it can obstruct the urethra and create resistance to urine flow. These circumstances force the bladder to work harder to move urine past that resistance.
This condition becomes increasingly common as men age. The Cleveland Clinic explains:
- About half of men with a prostate show some signs of BPH at 60 years old.
- By 85 years old, roughly 90% of men with a prostate show signs of BPH.
The precise cause of BPH is not completely understood by the medical community. Potential causes include changes in hormone levels as the body ages.
Symptoms of BPH
BPH has several potential symptoms. Not everyone who experiences BPH will experience all of these issues. They can vary in intensity from one person to the next. Effective BPH medical treatment can help to address many of these symptoms, as well as their underlying cause.
BPH often causes a variety of urinary symptoms, among others. These include:
- Difficulty urinating
- Straining to empty the bladder
- Nocturia (or waking up at night to urinate)
- A weak stream
- Delayed onset of urination
- Starting and stopping the flow
- Incomplete emptying
- Sometimes urinary tract infections
Diagnosing BPH
Diagnosis of BPH centers on three areas, as noted by The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). They are personal and family medical history, a physical exam, and medical tests.
Personal and family medical history helps a physician understand a patient’s current situation and other potential factors related to symptoms. A physical exam, including a digital rectal exam, helps to assess the state of the prostate and surrounding tissue. Medical tests, like a prostate-specific antigen (PSA) test, can help identify abnormalities that indicate BPH, prostate cancer, or related issues.
Is BPH Life-Threatening? Does BPH Need to Be Treated?
BPH is benign, meaning it is not cancerous and won’t spread to other parts of the body. This condition is generally not life-threatening, either.
However, BPH can cause significant quality of life issues. If left untreated, it can lead to more serious medical concerns. These include kidney damage and bladder stones, UCLA Health explains.
If BPH affects your quality of life, it’s important to consider treatment and discuss options with a healthcare provider.
Reviewing Current Treatment Options for BPH
There are several currently used treatment options for BPH, ranging from observation to medication and surgery. Sometimes, changes in lifestyle can be enough to reduce symptoms to a tolerable level in mild instances of BPH.
However, each case of BPH is different. It’s important to understand available treatment options to make an informed decision about your health.
Active Surveillance
Active surveillance does not involve surgery or medication. Instead, it is used to monitor the state of the prostate when BPH symptoms are mild and not disruptive. Follow-up exams and testing are used to monitor potential disease progression.
Medications
A variety of medications can help to address the cause and symptoms of BPH. Some medications, like phosphodiesterase-5 inhibitors, act on the prostate itself to stop its growth or reduce its size. Others, like alpha blockers, help to relax muscles in the urinary tract.
Medications can lead to mild and severe side effects in some cases. Discussing potential side effects of medications prescribed to you with your healthcare provider is crucial.
Surgical Treatment Options
A variety of surgical treatment options are available to treat BPH. These include:
Transurethral Resection of the Prostate (TURP)
TURP utilizes a specialized tool called a resectoscope, inserted in the urethra, to remove excess prostate tissue. The resectoscope includes a camera, but it only provides limited visibility during the surgery.
This is a relatively invasive procedure. It generally involves removing at least part of the prostatic urethra.
HoLEP is similar to TURP, but more aggressive. The excised tissue is moved into the bladder during the procedure. It is then cut into smaller pieces and removed from the body at the end of surgery.
TURP is among the most common treatments for BPH and has proven its effectiveness. However, it has significant side effects that also need to be considered:
- Blood loss. Research published in the peer-reviewed Journal of Endourology notes significant blood loss during a TURP procedure.
- Retrograde ejaculation. Retrograde ejaculation refers to the movement of semen into the bladder instead of out of the body following orgasm. It is generally not painful or disruptive but can be undesirable. The Cleveland Clinic notes estimates of retrograde ejaculation following TURP range from 70-90%.
GreenLight Laser Therapy
GreenLight treatment for BPH centers on the use of a laser and a camera inserted into the urethra. Specifically, this prostate laser surgery option involves a very high-powered laser as compared to laser focal therapy for the prostate.
GreenLight laser therapy is a standard surgical treatment for BPH. It has proven effectiveness. However, the limited visibility of the camera inserted in the urethra only provides so much context for surgeons. This treatment essentially vaporizes the urethra within the prostate along with enlarged tissue.
Side effects of this treatment include the potential for significant blood loss, although usually less than TURP. There is also a notable risk of retrograde ejaculation following the procedure.
Rezum
Rezum uses water vapor to transfer thermal energy to and destroy enlarged prostate tissue. A physician punctures the urethra with the delivery device to release steam to the targeted areas.
Rezum treatment includes a camera inserted into the urethra to guide the process. However, visibility is limited to the area in front of that camera and the needle tip is not visible.
This relative lack of context limits physicians in terms of accuracy. They have to essentially take an educated guess as to how much steam needs to be released and where.
MRI-Guided Laser Prostate Ablation: A New Option for Treating BPH
One common factor among many BPH surgical treatment options is the limited real-time feedback available to physicians.
Urethral cameras provide some context, but do not offer a complete picture of the prostate during treatment. Similarly, a lack of real-time thermometry (i.e. temperature monitoring) limits visibility. Those restrictions may lead to reduced effectiveness and increased potential for side effects in some cases.
MRI-guided laser prostate ablation is an emerging alternative that utilizes real-time MRI guidance along with real-time thermometry. The laser is inserted through the rectum, as opposed to the urethra. The laser itself is a 15-watt device using a 980 nm wavelength laser that includes a flexible diffuser tip.
MRI-guided laser ablation uses that laser to target enlarged areas of the prostate. The heat generated by the laser ablates (i.e. destroys) the enlarged tissue.
The same type of laser is FDA-cleared to be used in the brain. That distinction underscores the precise nature of MRI-guided laser ablation.
That high level of precision, as well as the effects of the laser itself, help to avoid significant blood loss. Crucially, the ejaculatory ducts and prostatic urethra have lower risk of damage compared with the traditional approaches.
Precise targeting and real-time monitoring also help to reduce the potential for other side effects, such as retrograde ejaculation. The use of a protective cooling medium also supports reduced risk of side effects.
Overall, the result is a minimally invasive procedure with a reduced potential for side effects. The potential for retrograde ejaculation is significantly lower than traditional procedures, at about 15%. Similarly, the risk of erectile dysfunction is less than 5%.
This procedure is sometimes called laser focal therapy and, more commonly, focal laser ablation (FLA). Focal therapy is used for prostate cancer treatment as well as the treatment of BPH.
The MRI imaging and thermometry used in FLA provide more insight and feedback during the procedure. The physician can actively monitor the prostate and surrounding tissue throughout the process. That leads to a few important advantages:
- It’s possible to apply more energy over larger areas. Real-time monitoring of the area provides more control. The physician can effectively adjust the laser’s position, power, setting, and duration of use. In essence, effectively modulating the dose of treatment is much easier.
- That additional energy can be precisely targeted. MRI-guided laser prostate ablation helps physicians minimize the burning of tissue outside of the target area.
New Research Demonstrates the Effectiveness of MRI-Guided Laser Prostate Ablation
A recent medical study published in the peer-reviewed Journal of Vascular and Interventional Radiology sheds more light on this procedure. Our physicians, Dr. Ara Karamanian and Dr. Aaron Harman, ran the clinical trial and authored the study.
The study group included 10 men, nine of whom completed two years of follow-up review. Among those nine men, several statistically significant symptom improvements were found:
Patients’ International Prostate Symptom Score (IPSS), which measures the self-reported severity of BPH symptoms, dropped. On a scale of 0-37, IPSS scores fell (lower is better) from initial baseline measurements by a mean of:
- 17.5±4.3 at 2 months
- 18.4±4.2 at 4 months
- 17.5±4.1 at 6 months
- 20.1±5.8 at 24 months
Notable improvements were also seen in patients’ IPSS Quality of Life (IPSS QoL) scores. At 24 months post-operation, the mean change was a drop of 3.7±1.3 on a 0-7 scale (lower is better).
Similarly, BPH Impact Index scores dropped. This is another patient-reported metric that assesses changes in the impact and severity of BPH symptoms over time.
At 24 months post-operation, patient BPH Impact Index scores dropped by a mean of 7.7±2.0 points. That’s a notable improvement on a 0-13 scale.
Patients in this study also saw slight, but not statistically significant, mean improvement from their baseline Sexual Health Inventory for Men (SHIM) scores. Importantly, there was no significant drop in erectile function.
Overall, these findings represent durable and positive changes following focal therapy on the prostate. Most patients realized reduced overall symptoms of BPH, fulfilling their objective in seeking treatment.
Side Effects of MRI-Guided Laser Prostate Ablation
In this study, a minority of patients reported side effects.
A pair of patients developed urinary tract infections that were successfully treated with antibiotics. Two patients developed retrograde ejaculation, and one required a second catheter to resolve urinary retention.
According to the Society of Interventional Radiology Adverse Events Classification System 2017 Modification, these adverse events are all considered mild. Incontinence and impotence did not develop among any patients. Additionally, blood loss for all patients was minor.
Make an Informed Choice About Treating BPH
Learning about treatment options for BPH helps you make an informed choice about your health. As a pioneer in developing focal laser prostate ablation for BPH, we are happy to share the results of this recently accepted study and help you become more informed.
Interested in learning more about treating BPH? Request a consultation today.
NOTE: The information provided on this website is general medical information and does not establish a physician-patient relationship. Please discuss your particular situation with a qualified medical professional.