What is Prostate Cancer?
A Common Cancer in Men
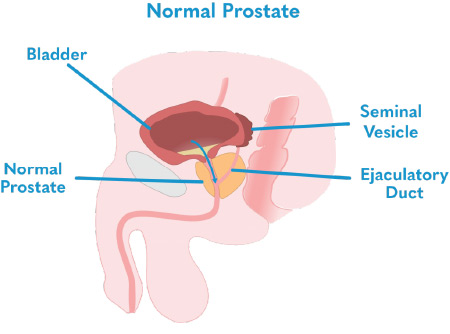
Prostate cancer happens when cells grow uncontrollably in the prostate gland. The prostate itself is a small gland located underneath the bladder and in front of the rectum. It contributes fluid to semen and helps to move semen through the urethra.
Many cases of prostate cancer are slow-growing and require minimal treatment. However, others are more aggressive, at risk of spreading quickly, and require treatment.
Approximately 1-in-8 men will be diagnosed with prostate cancer in their lifetime. It is the second most common form of cancer in men. More than half of cases occur in men over age 65. However, men in their late 40s are not immune to the disease.
Risk factors influence the likelihood of being diagnosed with prostate cancer. According to the American Cancer Society, these include age, family history, race (particularly non-Hispanic black men: 1 in 6 will be diagnosed), and obesity.
Research has shown that early diagnosis is key. Prostate cancer is highly treatable. It’s uncommon for men to suffer from life-altering effects due to prostate cancer if the condition is diagnosed early on and treated appropriately. Early detection and diagnosis help our experts determine the best treatment options for you.
Function of the Prostate Gland
The Anatomy of the Prostate
The prostate gland, approximately the size of a walnut, is only found in men. It surrounds the urethra; the tube which also carries urine from the bladder out of the body. It is located just below the bladder.
When the prostate enlarges as men age, the urethra is squeezed, making it difficult to urinate. The prostate gland is also part of the male reproductive system. Its purpose is to secrete a fluid that forms part of the seminal fluid, the fluid that carries sperm.
Neurovascular bundles run between a few millimeters, one-tenth an inch, from either side of the prostate. These bundles are delicate, 1-2 mm structures vital to erectile function.
Because of the close proximity, it is challenging to treat prostate cancer without destroying the neurovascular bundles. Millimeter precision is crucial to maintaining these nerves.
The prostate gland can grow as a man ages. An enlarged prostate sometimes causes no outwardly visible symptoms, but if not treated could impact long term urinary function.
Benign prostatic hyperplasia (BPH) shares some symptoms with prostate cancer, but is a distinct and separate condition. BPH can lead to serious complications if advanced cases are left untreated. However, BPH does not involve a risk of cancerous cells growing in the prostate or spreading in the body.
Symptoms of Prostate Cancer
Prostate cancer may have no noticeable symptoms in the early stages of the disease. As the cancer develops, symptoms often start to appear.
Many of these symptoms are related to urination. These include weak and intermittent urine flow, frequent urination, and difficulty with completely emptying the bladder. Some older men even get UTIs for the first time in their lives due to BPH.
People suffering from prostate cancer may also notice pain during ejaculation. Persistent pain in the body around the prostate is another potential symptom.
Grading Prostate Cancer
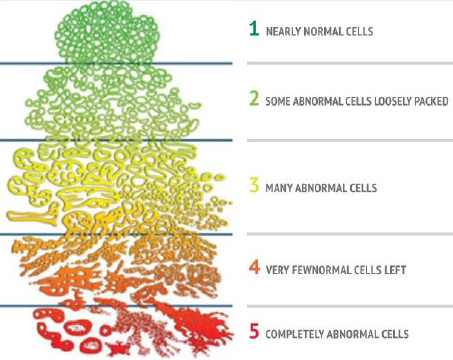
After a prostate-specific antigen (PSA) test, a digital rectal exam (DRE), and a recommended mpMRI indicate a likely prostate cancer diagnosis, a radiologist specializing in prostate imaging will attribute a PI-RADS score. Following a biopsy, a pathologist examines the cells under a microscope to determine how aggressive the tumor looks. A Gleason score is then assigned.
PI-RADS and Gleason Scores
PI-RADS stands for Prostate Imaging Reporting and Data System. It was designed by radiologists to help radiologists read a mpMRI and report the likelihood that a suspicious area contains clinically significant cancer. Each PI-RADS score indicates the likelihood to which significant prostate cancer (PCa) exists.
Gleason Scores were designed by a pathologist to identify five different patterns of prostate cancer and assign a grade to each. Your Gleason score will always be shown as the sum of two numbers, each ranging from 1-5 (e.g. 3+3 = total score of 6 or 4+3 = total score of 7). This set of numbers is based on the most aggressive patterns in each sample. Gleason Grade Groups are a newer way of describing the Gleason Score and they range from 1-5 instead of 6-10.
Physicians use the Gleason Score to help grade the severity of cancer and plan treatment. Each score aligns with a prostate cancer grade group.
Biopsy tissue is examined under a microscope, and the more aggressive the tissue appears the higher the Gleason Score.
Prostate Cancer: Questions to Ask Your Doctor
It’s important for every man to be armed with as much information about his current state of health and diagnosis. Each of the questions below can serve as talking points to guide the best course of treatment.
- How big is the tumor?
- What is my Gleason Score?
- How do my age and health affect the prostate cancer treatment I receive?
- Do I need treatment now?
- What are my prostate cancer treatment options?
- Am I a candidate for laser focal therapy, also known as FLA, or TULSA-PRO?
- What treatment options do you offer, and if I want to be evaluated for other options, should I speak with a different physician?
Prostate Cancer Treatment Options
There are three primary categories of treatment options for men diagnosed with prostate cancer:
- Active surveillance
- Invasive therapies
- Minimally invasive focal therapies
Prostate Laser Center performs laser focal therapy and TULSA-PRO minimally invasive procedures. Learn more about common prostate cancer treatment options.
Both procedures may be relevant treatment options for men with low- to medium-grade prostate cancer and even sometimes for high grade prostate cancer. However, every man is different, and so are their prostate concerns and treatment options.
References
[1] American Cancer Society. (n.d.). Key statistics for prostate cancer: Prostate cancer facts. Retrieved from https://www.cancer.org/cancer/prostate-cancer/about/key-statistics.html
